7 Common Reasons for Numbness in Your Hands
Table of Contents
- Overview
- 7 Most Common Hand Numbness Causes
- Common Reason #1: Hand numbness due to poor sleeping position
- How to fix a poor sleeping position
- Common Reason #2: Hand numbness from carpal tunnel syndrome
- How to fix carpal tunnel syndrome
►Steroid injections
►Myofascial release massage
►Carpal tunnel exercises
►Nocturnal bracing
- Common Reason #3: Hand numbness from diabetes-induced peripheral neuropathy
- How to fix diabetes-induced peripheral neuropathy
- Common Reason #4: Hand numbness from cubital tunnel syndrome
- How to fix cubital tunnel syndrome
►Cubital tunnel syndrome stretching exercises
►Cubital tunnel release surgery
- Common Reason #5: Hand numbness from thoracic outlet syndrome
- How to fix thoracic outlet syndrome
- Common Reason #6: Hand numbness from hand arm vibration syndrome
- How to fix hand arm vibration syndrome
- Common Reason #7: Hand numbness from cervical radiculopathy
- How to fix cervical radiculopathy
- Summary
- FAQs
- About
Overview
There are several reasons you may have numbness in your hands or fingers. In order to better understand the cause, it's necessary to consider 3 questions.
Do you have numbness in your hands all of the time or just occasionally? Is the numbness in the same areas or does it change location? Is your hand numbness worse at certain times?
The goal of asking yourself such questions is to force you to look more closely at the numbness. The answers to these questions can help pinpoint the cause.
Having numbness in your hands is not a rare problem. However, ANY numbness is abnormal. If you experience numb hands occasionally, perhaps once or twice per month, there’s probably not much to worry about. More than likely, you
slept in a position which strained your arm or wrist. This frequently causes numb hands upon waking up in the morning.
But having numb hands all (or most) of the time can indicate a more serious problem. If your hands are usually numb, or if you feel your hands going numb while performing a certain task, it means you probably have one of the 7 most common hand-numbing reasons listed here. They range from something simple (like a poor sleeping position) to more serious disorders (like carpal tunnel syndrome or diabetes). Each reason also outlines how you can FIX that problem.
7 Most Common Causes of Hand Numbness
Except for having a
stroke, numb hands alone are usually not life threatening. But the numbness should get your attention in order for you to understand its cause and how to fix the problem.
The 7 most common reasons for your hands going numb are described below. Also described is how to fix each problem.
From most to least common, the reason for having your hands go numb are:
- Poor sleeping position
- Carpal tunnel syndrome
(Click for easy & accurate self-test)
- Diabetes induced peripheral neuropathy
- Cubital tunnel syndrome
- Thoracic outlet syndrome
(Click for home self-test)
- Hand arm vibration syndrome
- Cervical radiculopathy
Less Common Reasons
Common Reason #1: Hand numbness due to poor sleeping position
How to fix a poor sleeping position
Don't cradle your head
Your head is heavy (10-12 pounds). Pressing its weight on your hand (palm up) or wrist joint for hours at a time will likely compress your ulnar or median nerve. So if you
must
sleep in that position, try putting a thin pillow between your head and hand.
Don’t over-bend your wrist joint
Unconsciously hyper-bending your wrist joint will pinch either the ulnar or median nerve (or both) at the wrist joint. To avoid this, wear a wrist brace at night. Be sure to wear a wrist brace
without a palmar spine. (A palmar spine will push into your carpal tunnel space and further damage your median nerve.)
Don’t push your elbows into the mattress
Sleeping on your back will almost certainly result in pushing your elbows into the mattress. This is especially true if you bend your elbow in order to rest your hands on your chest. The result may be a crushed ulnar nerve, resulting in morning numbness on the pinky side of your hand. For some people, changing their sleeping position is a radical adjustment. But
"sleep trainers" can help (see next). If you just can’t bear to change from back sleeping, try protecting your elbows instead. Soft, padded elbow protectors will help.
Use a "sleep trainer"
You can train yourself to sleep in a different position to avoid nerve compression.
This is called
sleep training.
You can use
one of several types of
sleep trainers to help. Training can be as simple as taping a tennis ball to your pajama back (to prevent rolling over and sleeping on your back). But more sophisticated electronic "alarm" devices are also available.
Common Reason #2: Hand numbness from carpal tunnel syndrome
You’re also at high risk of getting carpal tunnel syndrome if you:
Whichever reason brought the carpal tunnel syndrome, the reason you have numb hands is because the median nerve inside your wrist joint is trapped and pinched (or crushed) by swollen tendons.
The tendons are swollen due to irritation caused by
adhesionsbetween them. Therefore, the only way to effectively relieve symptoms is to remove the compression on the median nerve (i.e., "decompress" the nerve). This is the basis for
myofascial release massage.
How to fix carpal tunnel syndrome
Decompressing the median nerve by reducing swelling and inflammation is the only way to relieve finger or hand numbness (and other symptoms) of carpal tunnel syndrome. Nerve decompression can be achieved in one of two ways:
non-surgically or
surgically. Both methods can be quite effective, but obviously surgery is more aggressive.
Steroid injections
Steroid (or corticosteroid)
injections are often used by doctors to treat carpal tunnel syndrome. The reason is because steroids reduce tendon inflammation. That means as the tendons become less inflamed, they're not as swollen. Therefore, they don’t push against the median nerve as much, and symptoms lessen.
The problem with steroid injections is they only work on carpal tunnel syndrome about
45% of the time. Even then, their effects wear off in 3-6 months.
Over 60% of patients need another injection.
And therein is the second problem with steroid injections. Due to their
potential side effects, they should only be used a limited number of times. This is why steroid injections are considered a “temporary” remedy for carpal tunnel syndrome.
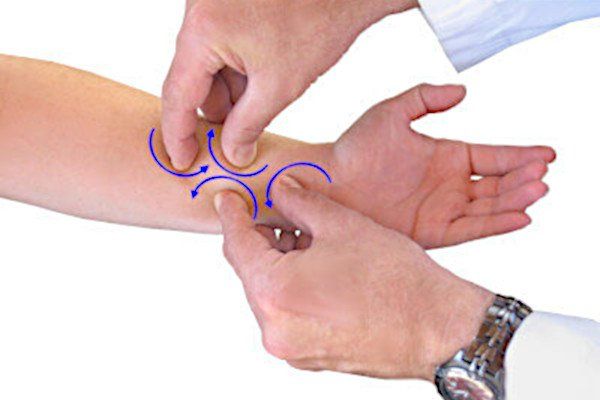
Myofascial release massage
Physical therapists, massage therapists, and chiropractors have been using
myofascial release massage to successfully treat carpal tunnel syndrome for decades. The reason it works so effectively is because of the
way
this massage is performed.
The practitioner kneads the tissues over the wrist joint. This action breaks apart adhesions on the tendons beneath. (It’s these adhesions which cause inflammation and swelling in the first place.) With daily massage, eventually the adhesions dissolve completely and the tendons are less swollen. That means they no longer push on the median nerve, and symptoms are eliminated.
The only downside to myofascial release massage is that it must be performed daily for 4-6 weeks, depending on how
severe your symptoms are. (A medical device called the
CarpalRx performs the myofascial release massage automatically, at home.)
Carpal tunnel exercises
Once again, the underlying problem in carpal tunnel syndrome is that adhesions between tendons cause them to become irritated and then swell. This swelling compresses the median nerve at the wrist joint.
However, specific
carpal tunnel stretching exercises (sometimes called “tendon gliding exercise”) directly attack those adhesions. In fact, the effect is similar to what myofascial release massage achieves (see above).
The 4 most effective carpal tunnel stretching exercises target the tendons as they pass through the carpal tunnel space inside the wrist joint. These are the
prayer stretch, stop stretch, finger interlace stretch, and
thumb stretch -
and can be found here.
Performing these exercises multiple times a day for several weeks can completely eliminate carpal tunnel syndrome. Of course, the more severe your condition, the more frequently you need to perform the exercises.
Nocturnal bracing
Nocturnal (night) bracing while you sleep is especially effective when carpal tunnel symptoms are still mild. More advanced symptoms might require nocturnal bracing
plus
other non-surgical remedies listed above.
Most people bend their hands while sleeping. This bending can pinch the median nerve. If you already have
signs of carpal tunnel syndrome, the nighttime bending can make the condition much worse. A
night brace (or splint) will keep your hand in the neutral position (i.e., straight) while you sleep. Continued use will lessen irritation and swelling. This lets the nerve decompress, and the symptom will resolve.
But be careful: not all braces will do. In fact, most wrist braces sold in pharmacies like CVS, Walgreens, Walmart, Rite Aid, etc.
can be harmful. If they have a
palmar spine, then the spine can press into your wrist joint and increase compression on the median nerve. Only
certified carpal tunnel braces have the supports on the sides of the wrist, not on the palm side.
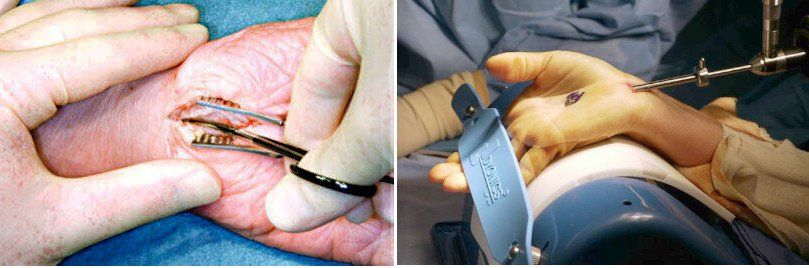
Open carpal tunnel release surgery
Open carpal tunnel release surgery means the surgeon makes a slit in your hand about 2-3 inches long. Then the surgeon cuts a ligament holding your wrist bones together. As the bones snap apart, they decompress the nerve trapped between them. The nerve decompression then relieves symptoms.
Endoscopic carpal tunnel release surgery
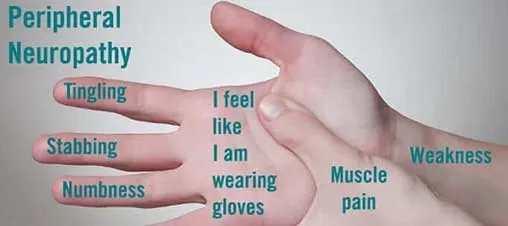
Common Reason #3: Hand numbness from diabetes-induced peripheral neuropathy
How to fix diabetes-induced peripheral neuropathy
Diabetes and peripheral neuropathy cannot be cured: you have them for life. But you can reduce your risk of having neuropathy by slowing the progression of diabetes. You can also lessen the effects of the nerve damage with certain
medicines.
Decades of research has shown that the key to slowing progression is
good management of blood sugar. That means you can reduce your risk of neuropathy by maintaining a normal (or as close as possible) blood sugar level.
Talk to your doctor to determine the best
target range for your blood sugar. It will be based on certain factors such as your age, overall health, and how long you've had diabetes. In other words, your blood sugar levels must be
individualized.
Generally speaking, the
American Diabetes Association recommends the following target range for your blood sugar levels if you have diabetes:
- Before meals: 80 to 130 milligrams per deciliter (mg/dL)
- After meals: less than 180 milligrams per deciliter (mg/dL)
Common Reason #4: Hand numbness from cubital tunnel syndrome
How to fix cubital tunnel syndrome
As with carpal tunnel syndrome, the only treatment for numb hands is to free the ulnar nerve from being trapped and crushed by surrounding tissues. There are two ways to achieve this;
surgery
and
stretching exercises.
Cubital tunnel syndrome stretching exercises
As with carpal tunnel syndrome, an effective
non-surgical remedy for cubital tunnel syndrome is dedicated exercising. Cubital tunnel syndrome exercises focus on stretching and strengthening the elbow area.
There are 3 key
stretching and strengthening techniques:
range-of-motion exercises, muscle strengthening exercises,
and
nerve gliding exercises.
Most therapists suggest a combination of all 3 exercises applied simultaneously. When a combination regimen is used, symptoms of cubital tunnel syndrome will usually resolve within 6-8 weeks.
Open cubital tunnel release surgery
The surgery used to relieve cubital tunnel syndrome is called “ulnar nerve release surgery”. The "open" procedure requires the doctor making a 3-4-inch long incision on the inside part of your elbow. It enables the doctor to see and access the ulnar nerve and its surroundings. Then the surgeon cuts the
overlying ligament trapping and crushing the ulnar nerve. As soon as that happens, pressure on the nerve is relieved and symptoms begin to disappear.
Endoscopic cubital tunnel release surgery
This type of cubital tunnel syndrome surgery is called “ulnar nerve release surgery”. It means the doctor makes one or two small incisions in the same area. Then an endoscope is used to view the ulnar nerve and its surroundings. A special scalpel then cuts the ligament which covers (and crushes) the nerve.
These two techniques have their own
advantages and disadvantages. They involve varying potential complications, healing and recovery times, and length or degree of post-surgical pain.
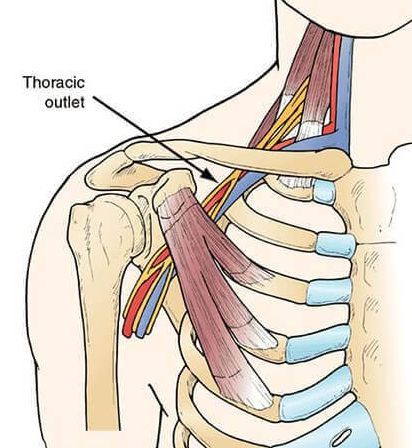
Common Reason #5: Hand numbness from thoracic outlet syndrome
How to fix thoracic outlet syndrome
There are 2 methods to treat thoracic outlet syndrome;
non-surgical
and
surgical. The most common thoracic outlet syndrome (neurogenic) is almost always treated successfully and permanently with
physical therapy exercises.
However, if physical therapy fails, neurogenic thoracic outlet syndrome can be treated surgically. The surgery is rather
aggressive. It involves removal of muscle tissue and/or the first rib.
In contrast, venous thoracic outlet syndrome is initially treated with
blood thinning drugs. Once the blood clot dissolves, the patient may need surgery to correct the underlying anatomical problem which caused the clot so it doesn’t reoccur.
Arterial thoracic outlet syndrome can
only be treated surgically. The doctor must remove the first rib and surrounding tissue.
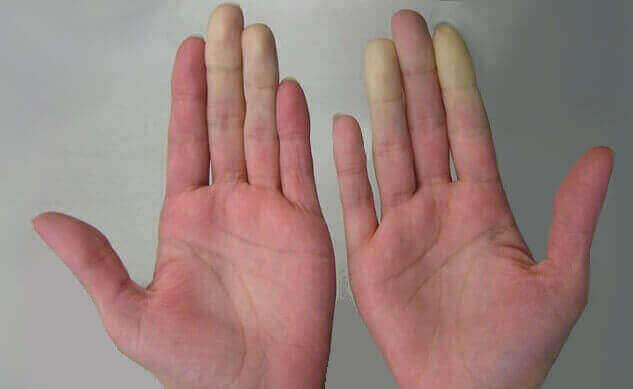
Common Reason #6: Hand numbness from hand arm vibration syndrome
How to fix hand arm vibration syndrome
Hand arm vibration syndrome a chronic and progressive disorder which usually takes years of vibrating tool use to fully develop. To keep it from occurring, you must
curtail or stop using the vibrating tools. Or at the very least, fully protect your hands (see below).
Unfortunately, in its advanced stages, hand arm vibration syndrome is
not reversible. This means that once hand arm vibration syndrome progresses to a certain point, you will lose most of your hand function. Necrosis (death of tissue, like skin) in the fingers will very likely result. This is why
prevention
of HAVS is crucial.
The National Health Service (UK) provides
comprehensive guidance for preventing HAVS. It focuses on minimizing risk, and makes a number of recommendations.
The most important recommendation is that workers in high risk occupations (i.e., those using vibrating tools) must be
proactive and take precautions.
One of these is to seek alternative work methods to eliminate or reduce exposure to vibration, such as using automated tools. Another recommendation is to exchange tools for those which produce less vibration. Also workstation schedules can change to limit a worker’s exposure to vibration.
Finally, and perhaps the easiest and most effective recommendation to implement, is to use well-padded, insulated gloves. This simple yet effective fix can protect against vibration and also keep the workers’ hands warm (since cold temperature exacerbates HAVS).
Common Reason #7: Hand numbness from cervical radiculopathy
How to fix cervical radiculopathy
There’s good news here. For most people, cervical radiculopathy will respond quite well to
conservative treatment. That means instead of surgery, medication and/or physical therapy will relieve symptoms. For many patients, pain and numbness will disappear relatively quickly (days or weeks). Other patients may need more time.
The first treatment of choice for cervical radiculopathy is wearing a
soft cervical collar. This is allows your neck muscles to rest and avoid strain. Doing so helps limit pinching at the nerve root when your neck moves. However, prolonged wearing of a collar should be avoided so that neck muscle strength is not compromised.
Physical therapy exercises
can also help resolve symptoms. These include exercises to strengthen your neck muscles and improve your neck’s range of motion. Sometimes
traction can be used to gently stretch the neck’s joints and muscles.
Certain medicines can also help relieve cervical radiculopathy. Nonsteroidal anti-inflammatory drugs (NSAIDs) like aspirin, naproxen, and ibuprofen can relieve inflammation and provide pain relief.
If these measures don’t provide good results,
steroids can be injected near the nerve to decrease inflammation.
Summary
When it comes to numbness in your hands, there are 7 likely candidate conditions that can cause the problem. Some are more severe than others. For most conditions, however, treatment for numbness in the hands involves non-surgical management, although in some instances surgery may be necessary.
FAQs
- What if none of these reasons explains the numbness in my hands?
Don't wait to see your doctor for a more thorough examination. The problem could be serious.
- Is it possible to have more than one hand numbing problem at the same time?
Yes. Many of the reasons listed can occur simultaneously; called a comorbidity. For instance, it's not unusual for a patient to have carpal tunnel syndrome as well as thoracic outlet syndrome or cubital tunnel syndrome.
- Does having numb hands only occasionally qualify it as needing attention?
It's best to talk with your doctor. He/she will give you a through check-up and determine if the problem is serious.
About