11 Causes of Hand Weakness
Table of Contents
Overview
Introduction
- Arthritis in the hands
- Ganglion cyst
- Sarcopenia
- Thoracic outlet syndrome
- Carpal tunnel syndrome
- Cubital tunnel syndrome
- Stroke
- Peripheral neuropathy
- Pinched cervical nerve (cervical radiculopathy)
- Epicondylitis
- Multiple sclerosis
Summary
FAQs
About
Overview
Have you noticed any hand weakness? Are your hands getting weak for no reason? Do you have weak hands now compared to say, a year ago? If so, there might be something serious happening.
Aging, of course, usually results in
loss of muscle mass. It’s related to a less active lifestyle most people have with increasing age. That means you no longer use your muscles as vigorously. As a result, normal aging results in generally weaker hands, arms, legs, etc.
But something else may be happening if the loss in your hand strength is noticeably greater than overall weakness elsewhere in your body. And it could be especially concerning if you experience
sudden
hand weakness. Weak hands might be a sign of an underlying disorder which needs attention now.
Introduction
The following are the top 11 main causes of hand weakness. They're listed in order of
most-to-least common disorders that might result in your hands feeling weak. Each one is discussed in detail below. They are:
1. Arthritis
2. Ganglion cyst
3. Sarcopenia
4. Thoracic outlet syndrome
(Complimentary self-test for thoracic outlet syndrome)
5. Carpal tunnel syndrome
(Complimentary self-test for carpal tunnel syndrome)
6. Cubital tunnel syndrome
7. Stroke
8. Peripheral neuropathy
9. Pinched cervical nerve (cervical radiculopathy)
10. Epicondylitis
11. Multiple sclerosis
1. Arthritis in the hands
(prevalence 16% male, 21% female)
The
Arthritis Foundation says there are over 100 different and distinct
types of arthritis. The
most common types are
osteoarthritis and rheumatoid arthritis. Essentially, they refer to a "wear and tear" disorder compared to an autoimmune disease, respectively.
Arthritis symptoms include:
- Pain at or near the affected joint
- Warmth at or near the affected joint
- Hand weakness (loss of grip strength)
- Grinding feeling in the joint
- Redness or swelling
- Cysts under the skin
- Limited range of motion of the affected joint
Treating Arthritis
Treating arthritis is very much tailored to the patient’s needs. This case-by-case approach to treatment should be discussed with your doctor. Treatment options may include any of the following:
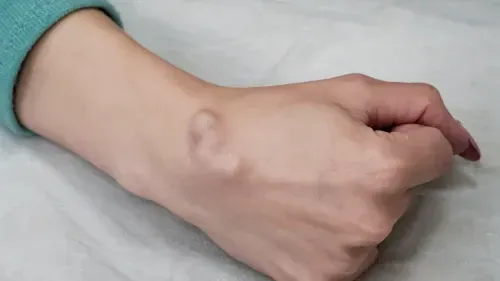
2. Ganglion cyst
(prevalence 19%, primarily in women)
A
ganglion cyst is a nodule that usually forms near a tendon or joint. The cyst is generally filled with jelly-like fluid. A ganglion cyst is the most common form of a lump or bump on the hand.
Ganglion cysts generally form on the back (knuckle side) of the hand. They are also benign. Sometimes, if the cyst is pressing on a nerve, it can result in hand weakness, pain, or tingling. However, this is not a common occurrence.
Symptoms of a ganglion cyst include:
- Moveable lump, usually on the back of the hand, near a joint
- Sometimes the lump is painful
- The lump can be so painful that it causes
hand weakness
Treating Ganglion Cysts
Most ganglion cysts will
resolve on their own without treatment. But if the cyst is painful, you can treat it by using one of the following
options:
- Pain medicines:
You can manage the pain from a ganglion cyst with
NSAID medicines like Advil, Aleve, Tylenol.
- Immobilization: Moving your hand can make the cyst bigger. This, in turn, can exert more pressure on a nerve and produce more pain. Immobilizing your hand with a wrist and hand brace can relieve the pain.
- Aspiration: Your doctor can remove fluid from inside the cyst. This remedy is used when the cyst is large or causing intense pain.
- Excision:
Your doctor may elect to completely remove the cyst if the above methods fail to provide relief.
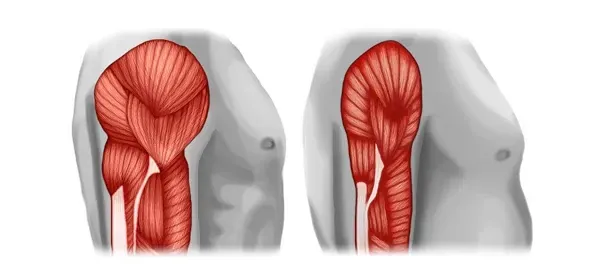
3. Sarcopenia
(prevalence 5-10% over age 65)
Sarcopenia means you are losing muscle mass. With loss of muscle mass comes weakness and decreased muscle function, like loss of hand strength. Sarcopenia can occur naturally with increasing age and inactivity. However, it can also result from:
Symptoms of sarcopenia may include:
- Unstable balance
- Trouble climbing stairs
- Muscle weakness
- Decreased endurance
- Reduced muscle size
Treating Sarcopenia
The options to treat sarcopenia center around
preventing and managing muscle loss. This can be achieved with physical activity, especially using resistance training. Increasing a muscle's mass improves its strength.
If sarcopenia is due to other disorders (like COPD, for instance), your doctor will address the underlying disorder. Then your doctor will recommend ways to increase your muscle mass based on your overall
treatment plan.
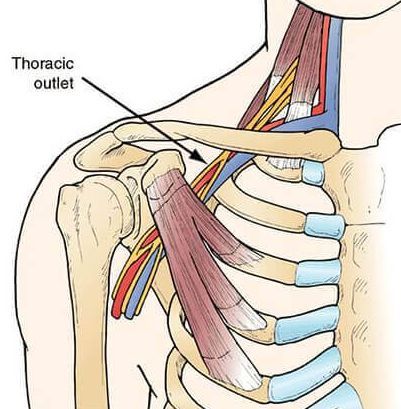
4. Thoracic outlet syndrome
(prevalence 8%)
Thoracic outlet syndrome is probably the most common disorder you never heard of. Yet if affects a
large proportion of the population.
Thoracic outlet syndrome occurs when the normally-open space between your collarbone and first rib begin to close down. This in turn squeezes on nerves, blood vessels, and muscles passing through the space.
Nerve compression makes up about 90% of thoracic outlet syndrome cases.
Most times, the cause of thoracic outlet syndrome is unknown. However, your chances of getting it are greater after a car accident or while performing repetitive movements.
Symptoms
of thoracic outlet syndrome depend on whether a nerve or blood vessel is compressed. They may include:
- Pain in the neck, shoulder, arm, or hand
- Numbness in the fingers and forearm
- Hand weakness
- Arm swelling and redness
- Arms and hands feel cold to the touch
- Arms and hands get easily fatigued
Treating thoracic outlet syndrome
Most cases of thoracic outlet syndrome are easily treated. The most common (and easiest) way to do so is with
stretching exercises. Certain exercises target the thoracic area. They loosen up the constricted outlet, thereby relieving pressure on the nerves and blood vessels passing through it.
5. Carpal tunnel syndrome
(prevalence 3%-6%)
This is perhaps the most commonly known of the various disorders causing hand weakness.
Carpal tunnel syndrome is actually a neurological disorder caused by
inflamed tendons.
When the hand and fingers are overworked (like repetitively performing grip and release motions) the flexor tendons in the forearm can become irritated and inflamed. That inflammation and swelling exerts pressure against the
median nerve.
Essentially, the nerve gets “trapped” inside the wrist joint. (This is why it’s called an “entrapment neuropathy”.) As a result, the nerve responds (reacts) and produces the characteristic symptoms of carpal tunnel syndrome.
Symptoms of carpal tunnel syndrome may include:
Treating carpal tunnel syndrome
Treatment options for carpal tunnel syndrome depend on
which stage of the disorder you have. Early or “mild stage” carpal tunnel can be treated effectively with pain medicines,
night braces, and
daily stretching exercises. Also, avoid harmful hand and finger activities (see this list).
More advanced stages of carpal tunnel syndrome (“moderate” or
“severe” stages) require more aggressive therapy. Usually,
all of the above therapies would be used in addition to daily
myofascial release massage. If these fail to provide significant relief, then
carpal tunnel release surgery may be recommended.
6. Cubital tunnel syndrome
(prevalence 2-6%)
Cubital tunnel syndrome, like carpal tunnel syndrome, is an entrapment neuropathy. But in this instance, the
ulnar nerve becomes trapped at the elbow. The reasons for entrapment are considered similar to that which happens in carpal tunnel syndrome. That is, over-use and
repetitive stress (strain) of the tendons at the elbow joint.
Symptoms of cubital tunnel syndrome include:
- Hand numbness and pinky finger numbness, especially when the elbow is bent
- Weak hands and fingers
- Pain in the hand
- Weak grip strength
- Finger coordination difficulties
- Pain on the inside area of the elbow
Treating cubital tunnel syndrome
7. Stroke
(prevalence 3%)
A
stroke occurs when a blood vessel in the brain is blocked or bursts. This diminishes the oxygen to the brain cells in that area, causing them to malfunction and often die.
Symptoms of stroke include:
- Since most strokes are silent, overt symptoms may not be apparent. Instead, patients feel a sudden headache, difficulty speaking, have balance or vision problems, and have numbness on one side of their body.
- Strokes can also cause numbness or
weakness
in the face, arm or leg, particularly on one side of your body.
- This well-known acronym applies to more overt signs of stroke:
FASTER. It means Face, Arms, Stability, Talking, Eyes, React.
F.A.S.T.E.R.
- Face: Drooping or numbness on one side of the face. When asked to smile, the smile is uneven.
- Arms:
When holding both arms high, one arm drifts downward because one arm is weaker.
- Stability: Dizziness or difficulty staying balanced, walking, or loss of coordination.
- Talking: Inability to talk or slurred speech; difficulty being understood or understanding speech. Cannot repeat simple sentences.
- Eyes: Difficulty seeing out of one or both eyes. Double vision.
- React: Call 911 or get to a hospital immediately – even if symptoms disappear.
Note the time when symptoms first appeared.
Treating stroke
Stroke treatment depends on the type of stroke the patient has experienced. The most
common type of stroke is called ischemic stroke.
The
main treatment for an ischemic stroke is administering a drug called
“tissue plasminogen activator" or TPA. This breaks up blood clots which impede blood flow in the brain. Intravenous TPA must be given within
3 hours after symptoms first appeared.
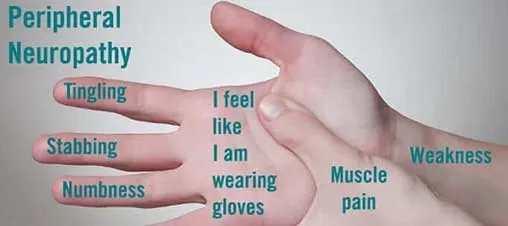
8. Peripheral neuropathy
(prevalence 1-7%)
Peripheral neuropathy can occur when
peripheral nerves (nerves of the limbs) become damaged. The nerve damage can occur:
- Metabolically, as with diabetes
- Chemically, as with Drug Induced Peripheral Neuropathy or
DIPN
- With
trauma, as when cutting, crushing or stretching the nerve
Symptoms
of peripheral neuropathy:
There are over
100 different kinds of peripheral neuropathy. The symptoms of each one depends on which nerve or nerves are affected. The
general symptoms include:
- Gradual onset of numbness or tingling in your hands or feet. This can spread into your legs and arms.
- Pain that's sharp, jabbing, burning or throbbing.
- Intense sensitivity to touching objects
- Pain when performing activities that normally don't cause pain, such as foot pain when putting weight on them or while under a blanket
- Poor coordination or falling
- Muscle weakness
- Sensation of wearing gloves or socks when you're not
- Motor nerve paralysis (when motor nerves are affected)
Treating peripheral neuropathy
Your doctor will recommend
treating
your peripheral neuropathy by addressing the underlying disorder. For instance, if the neuropathy is caused by diabetes, you and your doctor must work to keep your
blood glucose well-controlled.
In addition to treating the underlying disorder, neuropathy may be relieved in other ways. Many patients use pain relief medicines,
gabapentin
(a nerve pain reliever -
see warnings), braces,
massage, and
stretching exercises.
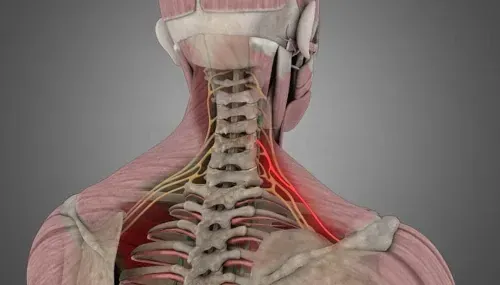
9. Pinched cervical nerve (cervical radiculopathy)
(prevalence 0.8%)
A pinched nerve (technically called
cervical radiculopathy) occurs when a structure (like a cervical bone, disc, or tumor) presses against a nerve exiting your cervical spine. The pressure causes irritation on the nerve which produces various symptoms.
Sometimes cervical radiculopathy
results from aging (called
cervical spondylosis). It can also occur from an injury, like a sudden trauma to the neck area which herniates a
cervical disc.
Symptoms of cervical radiculopathy include:
- Pain, usually starting in the neck which travels down your arm and into your hand
- Shoulder or hand weakness
- Hand or finger tingling
- Loss of sensation in the arms or hand
Treating cervical radiculopathy
Treatment for cervical radiculopathy depends on the severity of the disorder. Usually, although not always, realignment of the cervical spine is sufficient to reduce pressure on the pinched nerve. This can be achieved with a vertical collar, or with
traction.
Other treatments include using NSAID drugs like Advil, Aleve, or Tylenol. But if these methods do not help,
physical therapy may be needed. Physical therapy both loosens restrictions and strengthens neck muscles. Pain medicines and physical therapy can also be used in addition to
ketosteroid injections in the neck area.
Surgery is the last option when the above non-surgical remedies fail.
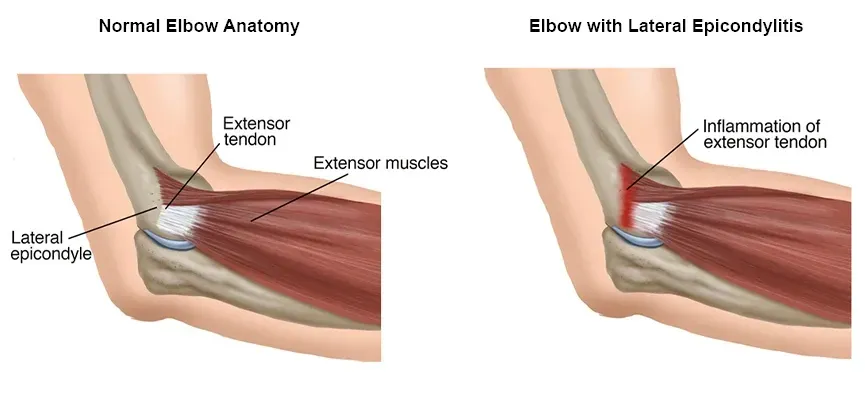
10. Epicondylitis
(prevalence 0.3%)
Epicondylitis can occur when tendons in the forearm near the elbow are damaged. There are two forms of epicondylitis: medial and lateral.
Medial epicondylitis (also called "golfer’s elbow") is an inflammation of the tendons that attach your forearm muscles to the
inside
of the bone at your elbow. These tendons bend your wrist toward your palm.
Lateral epicondylitis (also called as "tennis elbow") is an inflammation of the tendons that join the forearm muscles on the
outside of your elbow. These tendons bend your wrist away from your palm.
These disorders do not necessarily only result from playing golf or tennis. You can get epicondylitis from carrying heavy objects, repetitive activity, or extensive use of hand tools.
Symptoms of epicondylitis include:
- Pain on the inner forearm, from the wrist to the elbow
- Wrist and hand weakness
- Loss of grip strength
- Pain when squeezing a ball or bending your hand toward your little finger
Treating epicondylitis
The
first and best treatment for epicondylitis is avoidance. That means discontinuing the activity which caused the disorder to begin with. Continuing the activity will aggravate and worsen it. Other treatments include:
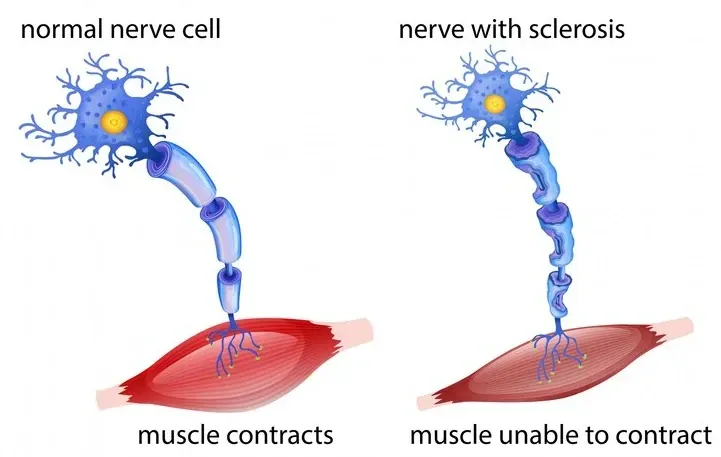
11. Multiple sclerosis
(prevalence 0.03%)
Multiple sclerosis is a relatively uncommon disorder affecting the
central nervous system (brain and spinal cord). Doctors and scientists are not certain what causes multiple sclerosis. However, the best evidence is that is an
autoimmune condition. This means your immune system attacks normally healthy nerves. The attack disrupts how the nerves perform.
Symptoms of multiple sclerosis
Multiple sclerosis can occur at any age, but onset usually occurs at 20 and 40 years old. Women are 3 times more likely have
relapsing-remitting multiple sclerosis. Some of the most common symptoms seen at the onset of multiple sclerosis include:
- Fatigue
- Vision problems
- Numbness and tingling in the limbs
- Muscle weakness (such as
hand weakness)
- Muscle spasms or stiffness
- Mobility problems
- Pain
- Problems thinking, planning, and learning
- Anxiety and depression
Treating multiple sclerosis
There is
no cure for multiple sclerosis. However,
physical therapy and
medications which suppress the immune system can help with these symptoms. They can also help slow the progression of the disease.
Summary
Weak hands can be a normal part of aging. However, extreme hand weakness or sudden onset of weak hands can be a sign of a more serious condition. If your hands are getting weak, one of the 11 disorders described here can be the cause. Discuss these with your doctor to obtain a proper diagnosis.
FAQs
- What if I can't identify the cause of my hand weakness?
You should consult with your doctor for thorough diagnosis. The problem could be serious and may require immediate medical attention.
- Can hand weakness come and go?
It's possible that hand weakness can come and go for an extended period of time. But the reason may be more related to how you use or hold your hand (e.g., at a particular angle or position).
- Which disorder causing hand weakness is the worst to have?
The the worst disorders to have are those with no cure, like stroke and multiple sclerosis.
About